United Nations Office on Drugs and Crime. World Drug Report 2024. (2024).
Connor, J. P. et al. Cannabis use and cannabis use disorder. Nat. Rev. Dis. Prim. 7, 16 (2021).
Lopez-Quintero, C. et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend. 115, 120–130 (2011).
Leung, J., Chan, G. C. K., Hides, L. & Hall, W. D. What is the prevalence and risk of cannabis use disorders among people who use cannabis? a systematic review and meta-analysis. Addict. Behav. 109, 106479 (2020).
European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2024: Trends and Developments. (Lisbon, Portugal, 2024).
Manthey, J., Freeman, T. P., Kilian, C., López-Pelayo, H. & Rehm, J. Public health monitoring of cannabis use in Europe: prevalence of use, cannabis potency, and treatment rates. Lancet Reg. Health Eur. 10, 100227 (2021).
Lees, R. et al. Psychosocial and pharmacological treatments for cannabis use disorder and mental health comorbidities: a narrative review. Psychol. Med. 51, 353–364 (2021).
Hasin, D. S. et al. Prevalence and Correlates of DSM-5 Cannabis Use Disorder, 2012-2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am. J. Psychiatry 173, 588–599 (2016).
Mongan, D. et al. Comparing cannabis use disorder in the general population with cannabis treatment seekers using multi-source national datasets: who receives treatment?. Eur. Addict. Res. 28, 103–112 (2022).
Courtney, K. E., Mejia, M. H. & Jacobus, J. Longitudinal studies on the etiology of cannabis use disorder: a review. Curr. Addict. Rep. 4, 43–52 (2017).
Hayatbakhsh, M. R., Najman, J. M., Bor, W., O’Callaghan, M. J. & Williams, G. M. Multiple risk factor model predicting cannabis use and use disorders: a longitudinal study. Am. J. Drug Alcohol Abus. 35, 399–407 (2009).
Butterworth, P., Slade, T. & Degenhardt, L. Factors associated with the timing and onset of cannabis use and cannabis use disorder: results from the 2007 Australian National Survey of Mental Health and Well-Being. Drug Alcohol Rev. 33, 555–564 (2014).
Marmet, S., Studer, J., Wicki, M. & Gmel, G. Cannabis use disorder trajectories and their prospective predictors in a large population-based sample of young Swiss men. Addiction 116, 560–570 (2021).
Hines, L. A. et al. Adverse childhood experiences and adolescent cannabis use trajectories: findings from a longitudinal UK birth cohort. Lancet Public Health 8, e442–e452 (2023).
Kosty, D. B., Seeley, J. R., Farmer, R. F., Stevens, J. J. & Lewinsohn, P. M. Trajectories of cannabis use disorder: risk factors, clinical characteristics and outcomes. Addiction 112, 279–287 (2017).
Myers, B., McLaughlin, K. A., Wang, S., Blanco, C. & Stein, D. J. Associations between childhood adversity, adult stressful life events, and past-year drug use disorders in the National Epidemiological Study of Alcohol and Related Conditions (NESARC). Psychol. Addict. Behav. 28, 1117–1126 (2014).
Vatansever, D., Wang, S. & Sahakian, B. J. Covid-19 and promising solutions to combat symptoms of stress, anxiety and depression. Neuropsychopharmacology 46, 217–218 (2021).
Li, L. Z. & Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 291, 113267 (2020).
Luo, M., Guo, L., Yu, M., Jiang, W. & Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – A systematic review and meta-analysis. Psychiatry Res. 291, 113190 (2020).
Xiong, J. et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 277, 55–64 (2020).
Pierce, M. et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7, 883–892 (2020).
Robinson, E., Sutin, A. R., Daly, M. & Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect Disord. 296, 567–576 (2022).
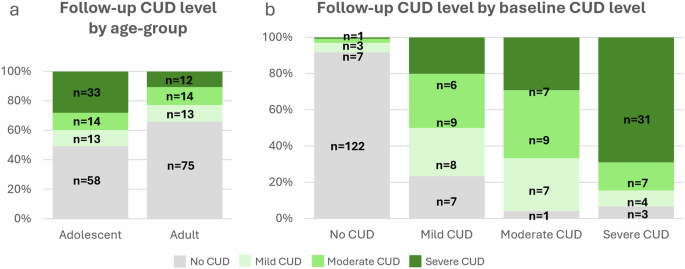
Jones, D., Freeman, T. P., Skumlien, M. & Lawn, W. Which factors are associated with Cannabis Use Disorder?: A One-Year Follow-Up Study, https://osf.io/eg2wq/ (2024).
Cousijn, J., Kuhns, L., Filbey, F., Freeman, T. P. & Kroon, E. Cannabis research in context: The case for measuring and embracing regional similarities and differences. Addiction 119, 1502–1504 (2024).
Cozier, G. E. et al. Synthetic cannabinoids consumed via e-cigarettes in English schools. medRxiv, 2024.2008. 2012.24311617 (2024).
Fataar, F. & Hammond, D. The Prevalence of Vaping and Smoking as Modes of Delivery for Nicotine and Cannabis among Youth in Canada, England and the United States. Int. J. Environ. Res. Public Health 16 https://doi.org/10.3390/ijerph16214111 (2019).
Hindocha, C., Freeman, T. P., Ferris, J. A., Lynskey, M. T. & Winstock, A. R. No smoke without tobacco: a global overview of cannabis and tobacco routes of administration and their association with intention to quit. Front Psychiatry 7, 104 (2016).
Chandra, S. et al. New trends in cannabis potency in USA and Europe during the last decade (2008-2017). Eur. Arch. Psychiatry Clin. Neurosci. 269, 5–15 (2019).
Potter, D. J., Hammond, K., Tuffnell, S., Walker, C. & Di Forti, M. Potency of Δ(9) -tetrahydrocannabinol and other cannabinoids in cannabis in England in 2016: Implications for public health and pharmacology. Drug Test. Anal. 10, 628–635 (2018).
Office for National Statistics (ONS). Drug misuse in England and Wales: year ending March 2024. (2024).
Office for Health Improvement & Disparities (OHID). Adult substance misuse treatment statistics 2022 to 2023: report. (2023).
Lawn, W. et al. cannTEEN: How does long-term cannabis use affect teenagers’ and adults’ cognition, mental health and brains? https://osf.io/jg9qp (2020).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59, 22–33 (1998).
Lecrubier, Y. et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur. Psychiatry 12, 224–231 (1997).
Robinson, S. M., Sobell, L. C., Sobell, M. B. & Leo, G. I. Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychol. Addict. Behav. 28, 154–162 (2014).
Petrilli, K. et al. Enhanced cannabis timeline followback (EC-TLFB): Comprehensive assessment of cannabis use including standard THC units and validation through biological measures. Addiction 119, 772–783 (2024).
Bohn, M. J., Babor, T. F. & Kranzler, H. R. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J. Stud. Alcohol 56, 423–432 (1995).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84, 791–799 (1989).
Borland, R., Yong, H. H., O’Connor, R. J., Hyland, A. & Thompson, M. E. The reliability and predictive validity of the Heaviness of Smoking Index and its two components: findings from the International Tobacco Control Four Country study. Nicotine Tob. Res. 12, S45–S50 (2010).
Brugha, T., Bebbington, P., Tennant, C. & Hurry, J. The List of Threatening Experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol. Med. 15, 189–194 (1985).
van der Pol, P. et al. Predicting the transition from frequent cannabis use to cannabis dependence: a three-year prospective study. Drug Alcohol Depend. 133, 352–359 (2013).
Chen, H., Cohen, P. & Chen, S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun. Stat.—Simul. Comput.® 39, 860–864 (2010).
Hmisc: Harrell Miscellaneous v. 5.1-3 (2024).
Chen, C.-Y., O’Brien, M. S. & Anthony, J. C. Who becomes cannabis dependent soon after onset of use? Epidemiological evidence from the United States: 2000–2001. Drug Alcohol Depend. 79, 11–22 (2005).
Chen, C.-Y., Storr, C. L. & Anthony, J. C. Early-onset drug use and risk for drug dependence problems. Addict. Behav. 34, 319–322 (2009).
Ehlers, C. L. et al. Cannabis dependence in the San Francisco Family Study: age of onset of use, DSM-IV symptoms, withdrawal, and heritability. Addict. Behav. 35, 102–110 (2010).
Le Strat, Y., Dubertret, C. & Le Foll, B. Impact of age at onset of cannabis use on cannabis dependence and driving under the influence in the United States. Accid. Anal. Prev. 76, 1–5 (2015).
Lawn, W. et al. The CannTeen Study: Cannabis use disorder, depression, anxiety, and psychotic-like symptoms in adolescent and adult cannabis users and age-matched controls. J. Psychopharmacol. 36, 1350–1361 (2022).
Lees, R. et al. Persistent increased severity of cannabis use disorder symptoms in adolescents compared to adults: a one-year longitudinal study. Eur. Arch. Psychiatry Clin Neurosci. https://doi.org/10.1007/s00406-024-01806-y (2024).
Lubman, D. I., Cheetham, A. & Yucel, M. Cannabis and adolescent brain development. Pharm. Ther. 148, 1–16 (2015).
Steinberg, L. Risk taking in adolescence: what changes, and why?. Ann. N. Y Acad. Sci. 1021, 51–58 (2004).
Maxwell, K. A. Friends: The Role of Peer Influence Across Adolescent Risk Behaviors. J. Youth Adolesc.31, 267–277 (2002).
DeWit, D. J., Adlaf, E. M., Offord, D. R. & Ogborne, A. C. Age at first alcohol use: a risk factor for the development of alcohol disorders. Am. J. Psychiatry 157, 745–750 (2000).
Chassin, L., Fora, D. B. & King, K. M. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effects of familial alcoholism and personality. J. Abnorm. Psychol. 113, 483–498 (2004).
Curran, H. V. et al. Which biological and self-report measures of cannabis use predict cannabis dependency and acute psychotic-like effects?. Psychol. Med. 49, 1574–1580 (2019).
Swift, W., Coffey, C., Carlin, J. B., Degenhardt, L. & Patton, G. C. Adolescent cannabis users at 24 years: trajectories to regular weekly use and dependence in young adulthood. Addiction 103, 1361–1370 (2008).
von Sydow, K., Lieb, R., Pfister, H., Höfler, M. & Wittchen, H. U. What predicts incident use of cannabis and progression to abuse and dependence? A 4-year prospective examination of risk factors in a community sample of adolescents and young adults. Drug Alcohol Depend. 68, 49–64 (2002).
Becker, J. B., McClellan, M. L. & Reed, B. G. Sex differences, gender and addiction. J. Neurosci. Res. 95, 136–147 (2017).
Zakiniaeiz, Y. & Potenza, M. N. Gender-related differences in addiction: a review of human studies. Curr. Opin. Behav. Sci. 23, 171–175 (2018).
Duncan, S. C. et al. Comorbidity and temporal relations of alcohol and cannabis use disorders from youth through adulthood. Drug Alcohol Depend. 149, 80–86 (2015).
Hindocha, C. et al. Associations between cigarette smoking and cannabis dependence: a longitudinal study of young cannabis users in the United Kingdom. Drug Alcohol Depend. 148, 165–171 (2015).
Cavalli, J. M. & Cservenka, A. Emotion dysregulation moderates the association between stress and problematic cannabis use. Front Psychiatry 11, 597789 (2020).
Cousijn, J., Kuhns, L., Larsen, H. & Kroon, E. For better or for worse? A pre-post exploration of the impact of the COVID-19 lockdown on cannabis users. Addiction 116, 2104–2115 (2021).
Cerdá, M. et al. Association between recreational Marijuana legalization in the United States and changes in Marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry 77, 165–171 (2020).
Leung, J., Chiu, C. Y. V., Stjepanović, D. & Hall, W. Has the Legalisation of Medical and Recreational Cannabis Use in the USA Affected the Prevalence of Cannabis Use and Cannabis Use Disorders?. Curr. Addiction Rep. 5, 403–417 (2018).
O’Grady, M. A., Iverson, M. G., Suleiman, A. O. & Rhee, T. G. Is legalization of recreational cannabis associated with levels of use and cannabis use disorder among youth in the United States? A rapid systematic review. Eur. Child Adolesc. Psychiatry 33, 701–723 (2024).